The hidden cost of plastic in healthcare
“I just want to say one word to you, just one word - plastics. There’s a great future in plastics.” These words voiced by the fictional character, Mr McGuire in the 1967 film, The Graduate, were truly prophetic as since 1950, plastic production has increased by a factor of 230 from 2 to 460 million tonnes per year. Whilst plastic has enabled innovation in many industries including healthcare, this has come at an environmental and social cost which cannot be ignored. 98% of plastic is derived from fossil fuels, the industry produces 2 billion tonnes of CO2 per year and almost 40% of products are intended for single use. Compared to today, production is predicted to double by 2040, triple by 2060 and we can neither get to ‘net zero’ nor restore the planet to good health without considering plastic.
Fossil fuel plastic
causes death,
disability, and disease at every stage of its lifecycle; impacting upon the
health of the planet
and the many species, including humans, which call it home. Plastic is
comprised of complex polymers and thousands of chemicals which can be
persistent, bio accumulative and toxic including endocrine disrupters, a particular
concern for the food and medical industries. Plastic is designed to be durable
and in 2018, it was reported that 6.3
of the 8.3 billion tonnes produced persists as waste in landfill or the
environment. Human health impacts are predominantly experienced by those in
lower Human Development Index countries, fence line communities, the vulnerable
and extremes of age.
Healthcare organisations
must be cognizant of their footprint; otherwise, the products and services procured
and used with good intention will, through contributing to climate change and
environmental ill health, fuel further demand for services at a time when they
themselves are trying to reduce their own environmental impact. It is therefore
welcome to see the NHS
Standard Contract requiring action to be taken by the whole value chain to
reduce the avoidable use of single use plastic which comprises 23%
of the waste produced by the NHS, most of which is ultimately incinerated
whether it sees clinical action or not.
The UNEP
Global Plastic Treaty aims to ‘turn off the tap’ on single-use plastics and
whilst healthcare may fall into the category of ‘essential
use’, we must still aim to first, do least harm by reducing
use whenever possible. Despite innovations in material science, bioplastic,
reduction in medical device plastic mass, use of less-toxic polymers, reintroduction
of reuseable products and recycling, we must be honest that for the foreseeable
future, healthcare will remain dependent on many single-use plastic products.
One of the most
important decisions a healthcare professional can make is when to open the
packaging of a single-use device as once opened, the item becomes waste whether
used or not. It’s therefore essential to move from a ‘just in case’ to a ‘confirmed
required’ mindset. Staff responsible for preparing clinical areas like
anaesthetic rooms must check the requirements of anaesthetists before items are
opened. An equally important decision is how to dispose of used items safely with
the least environmental harm. Healthcare waste is deemed non-hazardous until
proven or suspected otherwise and appropriate containers must therefore be available
to accommodate all potential waste types for the specific clinical area.
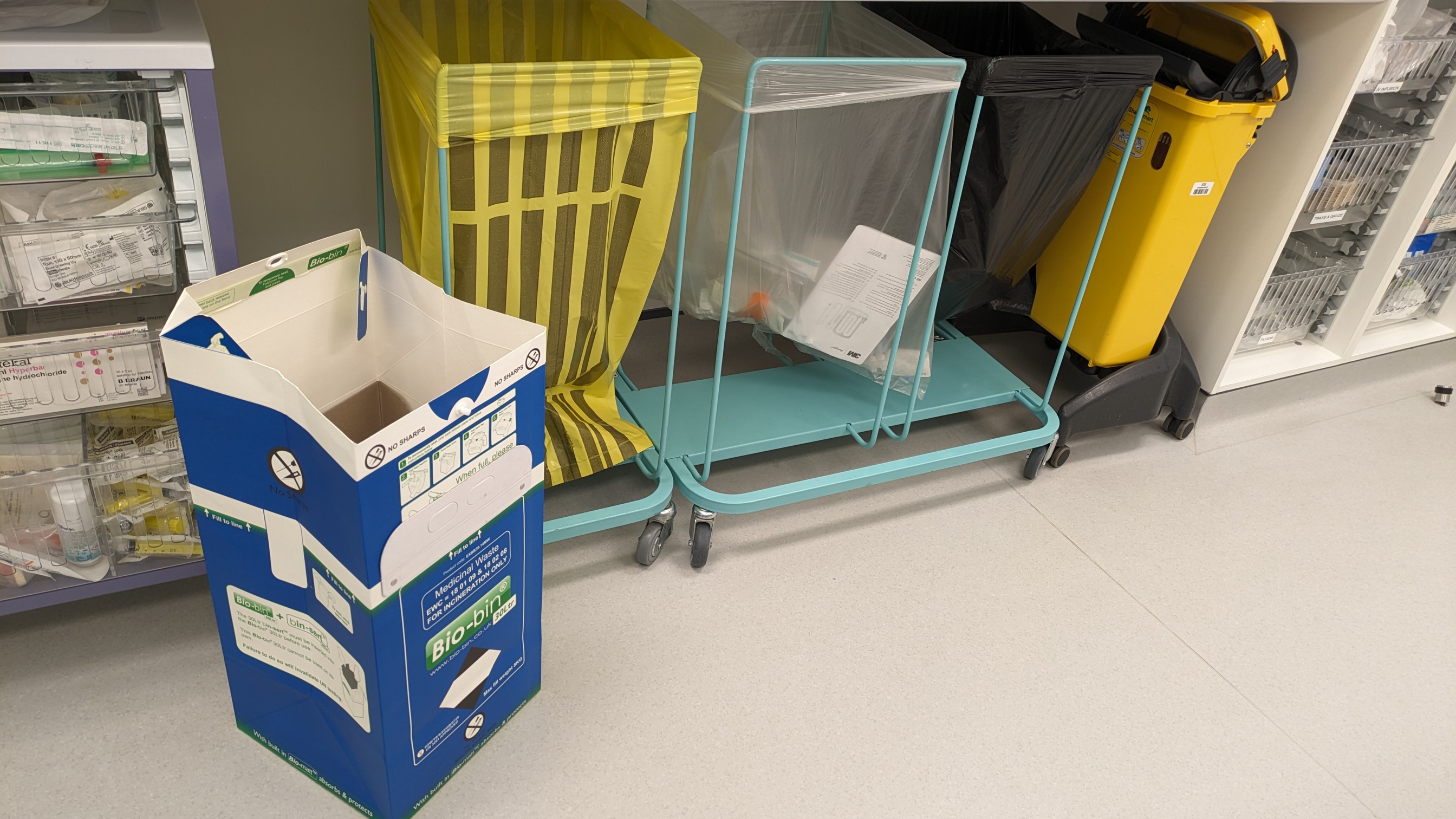
Safe
and sustainable management of healthcare waste provides clear guidance and its
essential clinical, sustainability and waste management leads create supporting
materials to help staff segregate waste correctly. Ensuring waste is disposed
through the correct waste stream using the most sustainable containers has a significant,
measurable impact on the amount of plastic consumed, distance transported,
method of treatment, whether the energy created can be utilised by the national
grid and cost.
Mapping these pathways
and calculating metrics for our different waste streams led to several changes.
By moving to Sharpsmart reuseable
sharps bins, our 11-bedded critical care unit reduced the amount of (single-use
sharp bin) plastic incinerated by 2.3 tonnes per year and through introducing blue Bio-bin containers into every bedspace,
redirected 6.4 tonnes of medicinal waste (predominantly used fluid bags,
syringes and giving sets) to the less environmentally harmful, non-hazardous waste
stream.
This waste
redirection followed an analysis of Health
and Safety Executive Regulations, a local risk assessment and agreement the
risk to staff from a giving set ‘spike’ which remained embedded in an
intravenous bag was minimal. We communicated that all giving sets along with
their attached bags of intravenous fluids/residual pharmaceuticals could be
disposed of in Bio-bins and since making this change several years ago, no
associated injuries have been reported. The only pharmaceuticals not disposed through
the blue waste stream are those with cytotoxic or cytostatic properties, hazardous
sharps, or items contaminated during use. These are placed in the purple or yellow
sharp waste streams respectively.
This ‘balance of
probabilities’ approach to theoretical harm from a shielded giving set
spike compared to the known increased environmental harm from overly
cautious classification of healthcare waste as hazardous is a great example of
a pragmatic approach to sustainability. Challenging existing processes which we
continue to do because we’ve “always done it that way” is essential when plotting
a path to truly sustainable healthcare. Concerns over the space required for these
additional waste containers were quickly allayed by the positive feeling arising
from a visible reduction of the environmental impact of care. Demands on staff
time reduced through fewer container exchanges and cost savings amounted to
thousands from just one clinical area.
Reducing the demand
pull for single-use items can be challenging if the infrastructure to support the
re-introduction of reuseable devices has changed and whilst supporting and pursuing
the principles of circularity, it’s essential to consider service demands and
patient needs. For example, a reuseable bronchoscope on critical care is of
little value when in transit for cleaning or being repaired which in our
experience, can take weeks. Every additional day a patient spends on the unit comes
with an energy, plastic,
drug and pollution cost; factors not always included in product life
cycle assessments. Our approach is therefore to ensure continued
availability of single
patient use bronchoscopes and to support environmentally-ambitious
companies in making devices as sustainable as possible.
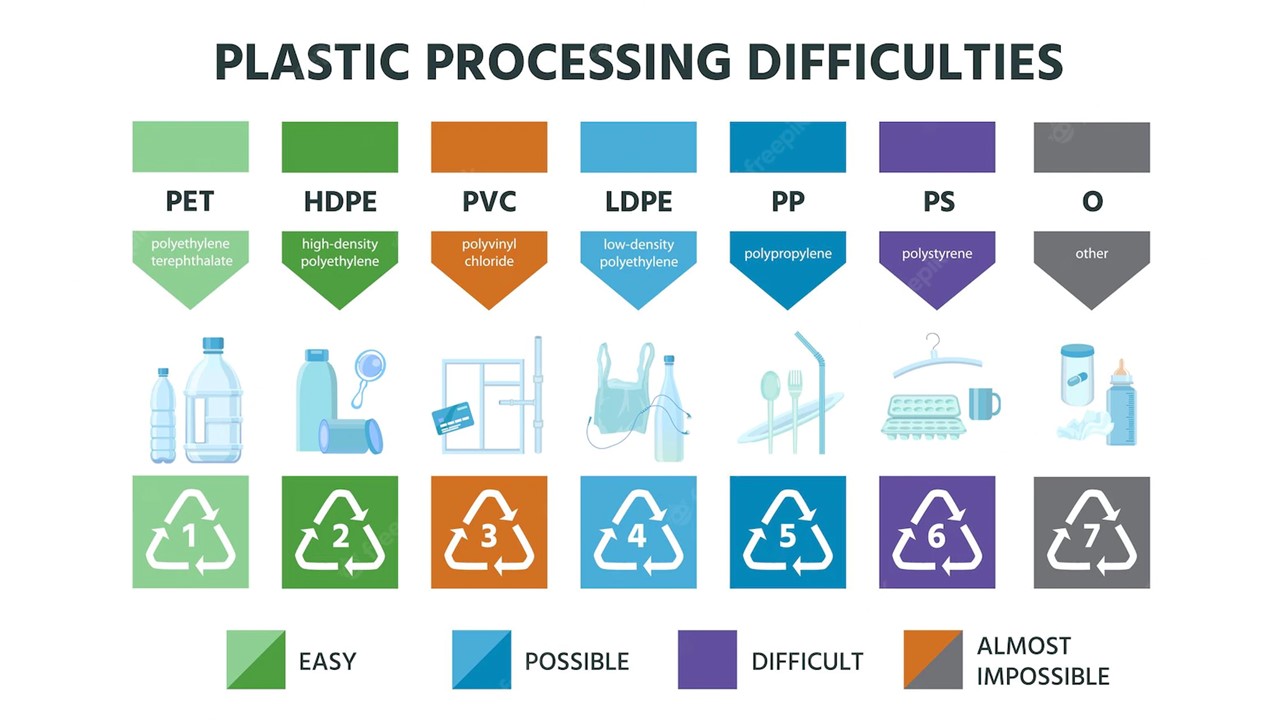
Despite the use
of composite materials and distinct lack of clues on packaging, we continue to
separate plastic from paper never sure what can or will be recycled. Whilst
items contaminated with a body fluid will primarily be directed toward the
offensive waste stream (tiger bin), questions are often asked of why we do not
recycle non-hazardous plastic waste. Is there evidence this poses a higher risk
than a random plastic drinks bottle destined for recycling following a beach
clean? As material complexity may currently preclude this pathway, future
products and packaging must be designed to be reused, recycled or disposed of
with minimal environmental impact whilst as an industry, we must be pragmatic
about risk.
My personal journey
exploring healthcare plastic and waste has thrown up all sorts of emotions.
Plastic is simultaneously harmful and beneficial, but with the benefits received
by those in countries with accessible healthcare system and the harms
externalised to the planet and those less fortunate. With the increased
knowledge we now possess, we should at least acknowledge the harm, use products
responsibly, communicate why, educate our peers and first, do least harm
whenever possible.
Everyone has an equal right to the highest attainable standard of physical and mental health and from a climate and environmental perspective, health is everything; it’s why we care. The trusted voices of healthcare professionals can, as we saw during the COVID-19 pandemic, cut through the noise and by including climate, environment and their impacts on health within our own professional development, we can become effective communicators inspiring others to act both in their personal and professional lives.
Richard Hixson.
Related Articles
How can I reduce my use of plastic in healthcare?
Fossil fuel plastic causes death, disability, and disease at every stage of its lifecycle; impacting upon the health of the planet and the many species which call it home. Whilst the global plastics treaty is taking shape, healthcare professionals can act now to reduce their own impact and educate others.
Written 08.05.2024
View Article

Climate and Environmental Literacy on CPDmatch
Why we need collaboration to improve climate and environmental literacy.
Written 23.11.2024
View Article
Achieving high staff engagement with net zero education and training in the NHS
The Delivering a net zero NHS statutory guidance, recognises that an upskilled workforce will be needed to drive and implement net zero initiatives. They will need to be supported to learn, innovate and embed sustainable development into everyday actions in the health service. This is how one UK Trust achieved high compliance in net zero training.
Written 03.08.2024
View Article
Aethic and the fight against Greenwashing: “reef safe” claims
Sun protection is essential, but with growing awareness about environmental impact, choosing the right sunscreen can feel overwhelming. Unfortunately, some brands exploit this concern with "greenwashing".
Written 25.05.2024
View Article
CPDmatch FAQs
The following Frequently Asked Questions (FAQs) are written with healthcare professionals in mind although many of the principles will be relevant to other professions. Please contact us if you have any comments or specific questions you’d like us to answer.
Written 03.06.2024
View Article